Extreme weather events, rising temperatures, and other climate changes are already shaking the foundations of healthcare. Hospitals face increased risks of power outages, facility damage, and resource scarcity, all while the demand for care rises due to climate-related illnesses and injuries. Healthcare systems must adapt quickly to protect patients and staff. This post will explore how climate change is reshaping hospital planning, resource allocation, and long-term strategies for maintaining care in an unpredictable future.
Understanding Climate Change and Its Effects on Health
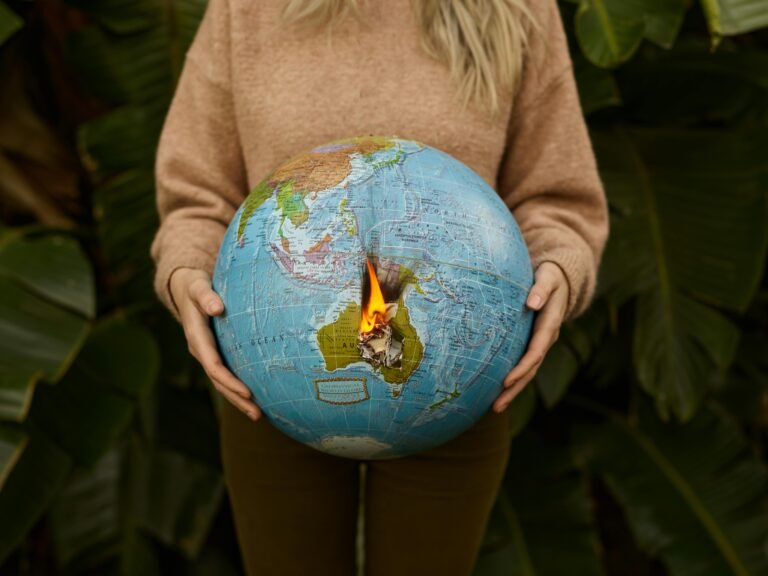
Climate change is becoming one of the most significant challenges of our time, not just for nature but also for human health. As the planet warms, extreme weather events, rising sea levels, and environmental disruptions are altering how we live, work, and stay healthy. The ripple effect on healthcare systems is undeniable, leaving no corner of society untouched in its wake.
Definition of Climate Change
Climate change refers to long-term shifts in weather patterns and average temperatures. These changes are largely driven by human activities like burning fossil fuels, deforestation, and industrial processes, which release greenhouse gases into the atmosphere. The result? A warming planet that disrupts ecosystems, weather cycles, and, ultimately, human lives. Think of it as nature’s alarm clock, and it’s ringing louder than ever.

Photo by ArtHouse Studio
Health Risks from Climate Change
Climate change isn’t just an abstract environmental issue; it directly impacts your health. It intensifies heatwaves, which can cause heatstroke and exacerbate heart and lung conditions. Air quality declines due to increased pollen and pollution, worsening asthma and other respiratory issues. Beyond that, flooding and storms increase waterborne diseases, while warming climates expand the ranges of disease-carrying insects like mosquitoes and ticks.
Consider this:
- Extreme heat: Linked to dehydration, heat exhaustion, and cardiovascular strain.
- Poor air quality: Aggravates asthma, bronchitis, and other lung diseases.
- Infectious diseases: Higher temperatures help mosquitoes spread diseases like malaria and dengue.
- Mental health: Displacement and climate-related disasters can lead to anxiety, depression, and trauma.
Each of these risks highlights the importance of urgent adaptation measures to shield global populations from harm.
Impact on Vulnerable Populations
Not everyone faces the same risks. Vulnerable populations—including children, the elderly, low-income communities, and those with pre-existing medical conditions—often bear the brunt of climate change. For instance:
- Children: Their developing immune systems make them more prone to diseases like heat-related illnesses or waterborne infections.
- Seniors: Age-related vulnerabilities can amplify the risks of extreme heat and respiratory conditions.
- Low-income communities: Economic limitations reduce their ability to adapt, such as affording air conditioning or relocating from flood zones.
- Pre-existing medical conditions: Individuals with diseases like asthma or heart issues are at higher risk when faced with worsening air quality or heatwaves.
Picture this: while one neighborhood rebuilds after a hurricane with insurance funds, another struggles to make ends meet. The disparity illustrates how climate change exacerbates systemic inequalities, forcing public health to play catch-up.
Long-Term Planning Needs for Hospitals
Climate change is pushing hospitals to rethink how they function, from their physical structures to the resources they depend on. The increasing frequency of extreme weather events, such as hurricanes, floods, and wildfires, underscores the importance of preparing for future challenges. Long-term planning requires hospitals to adapt their infrastructure, resource strategies, and emergency planning to ensure patient safety and operational continuity.
Infrastructure Vulnerability

Photo by Markus Spiske
Hospitals are not immune to the destructive effects of extreme weather. High winds can damage roofs and windows, flooding can destroy medical equipment, and wildfires can make facilities inaccessible. These vulnerabilities directly compromise patient care and staff safety.
- Flood risks: Coastal and low-lying hospitals are particularly at risk. Rising sea levels and heavy rainfall could overwhelm drainage systems and damage electrical systems located in basements.
- Storm-proofing needs: Facilities in hurricane-prone areas require reinforced windows and roofs to withstand strong winds.
- Wildfire exposure: Hospitals in drier regions may need improved air filtration systems to combat smoke and ash intrusion during wildfire seasons.
A proactive approach to structural upgrades can save lives. For example, elevating key infrastructure components, such as backup generators, above flood-prone areas is a practical step. Similarly, green building designs can help mitigate overheating in areas experiencing intense heatwaves.
Resource Allocation
Climate change is reshaping what hospitals need and how they secure their resources. Limited water, power outages, and interruptions in supply chains are becoming more common. Hospitals need adaptive strategies to manage these difficulties.
- Energy: Reliable backup power systems are no longer optional. Solar panels and microgrids can help reduce dependency on vulnerable regional power supplies.
- Water: Conservation strategies, like rainwater harvesting, can help mitigate shortages during droughts.
- Supplies: Stockpiling essential materials like personal protective equipment (PPE) and medications ensures readiness for extended disruptions.
By diversifying resource sources and adopting sustainable practices, hospitals can better handle climate-related shortages. It’s not just about saving money; it’s about saving lives when the unexpected happens.
Emergency Preparedness
Traditional emergency plans may no longer suffice in the face of climate risks. Hospitals need to account for more frequent and severe disasters. Emergency response protocols should evolve to reflect new challenges.
- Evacuation planning: Have plans for moving patients and medical equipment quickly in response to immediate dangers like floods or fires.
- Community integration: Collaborate with local emergency management agencies to prioritize high-risk populations.
- Training: Regular disaster simulations can familiarize staff with updated procedures, ensuring a faster and more effective response when it matters most.
Climate-focused emergency preparedness isn’t just an administrative task; it’s a critical safety measure. Hospitals must remain operational even under the most adverse conditions to fulfill their mission of care.
Hospitals hold an essential role during crises, providing a lifeline when communities are most vulnerable. Adapting their planning strategies to address climate impacts is not just prudent—it is imperative.
Adapting Healthcare Facilities
Climate change is forcing hospitals to rethink how they design buildings, use technology, and work with communities. Investing in smarter, sustainable strategies is no longer optional—it’s essential for keeping care accessible and safe.
Sustainable Design Principles

Photo by Jimmy Liao.
Hospitals must be designed to endure the stress of extreme weather while minimizing their environmental impact. Sustainable building practices create facilities that are more energy-efficient, adaptable, and resilient during crises.
Key sustainable design strategies include:
- Green rooftops and walls: Help regulate indoor temperatures and reduce urban heat island effects.
- Renewable energy systems: Solar panels and wind turbines ensure access to power during outages.
- Water management systems: Rainwater harvesting and low-flow plumbing conserve resources during droughts.
- Robust materials: Building with weather-resistant materials minimizes damage from floods, high winds, or fires.
Integrating these eco-friendly principles saves operational costs while protecting patients and infrastructure. Hospitals that invest in sustainability are better equipped to withstand the physical and financial toll of climate change.
Investment in Technology
Technology is redefining how hospitals prepare for and respond to climate challenges. Digital tools and data-driven systems enhance efficiency and care delivery, even when disruptions occur.
Hospitals can rely on innovations like:
- Early warning systems: Track storms, heatwaves, and other environmental risks to prepare in advance.
- Telemedicine: Maintains access to care for patients stranded during natural disasters.
- Renewable-powered backups: Microgrids and battery storage systems secure energy during grid failures.
- AI and predictive analytics: Monitor trends and anticipate supply shortages or staffing needs.
By prioritizing technology, hospitals can stay operational in unpredictable moments. Beyond preparation, tech integrates sustainability with smarter energy use and waste reduction strategies.
Community Health Initiatives
Hospitals don’t just serve patients inside their walls—they are anchors in their communities. Engaging with local residents ensures that climate adaptation extends beyond the building.
Simple yet impactful initiatives include:
- Community education: Teaching families about heat safety, water conservation, and emergency readiness.
- Partnerships with local groups: Collaborating with governments and nonprofits for disaster response or resource sharing.
- Mobile health clinics: Reaching underserved populations during extreme weather events.
Hospitals also benefit from involving community voices in resilience planning. Those partnerships strengthen trust and reduce risks for the most vulnerable populations, ensuring no one is left behind.
Adaptation isn’t just about the hospital—it’s about creating healthier, more prepared communities.
Policy and Regulatory Considerations
Addressing climate change in healthcare requires a coordinated approach, and this starts with policies that guide hospitals in adapting to new challenges. Governments, institutions, and private entities play a central role in ensuring that healthcare systems are resilient and prepared.
Health Policy Changes
Health policies need to evolve to address the realities of a changing climate and its impact on healthcare delivery. Regulatory frameworks must recognize that climate resilience is as essential as medical infrastructure.
Examples of necessary policy shifts include:
- Setting mandatory climate risk assessments for hospitals.
- Requiring climate adaptation plans as a condition for licensure or accreditation.
- Introducing sustainability goals, such as energy efficiency targets for healthcare facilities.
- Incentivizing the use of renewable energy sources in hospital operations.
The Health Sector Climate Pledge, initiated by the U.S. Department of Health and Human Services (HHS), is an example of a forward-thinking policy. It encourages health organizations to cut greenhouse gas emissions by 50% by 2030 and achieve net zero by 2050. These policies create a roadmap for transforming healthcare into a system that mitigates environmental risks while ensuring patient safety.

Photo by Leeloo The First
Funding and Financial Support
Adapting hospitals to climate challenges requires significant financial investments. Many healthcare systems lack the resources for large-scale improvements, leaving them vulnerable. Diverse funding sources are essential to bridge this gap.
Potential funding opportunities include:
- Federal Grants: Programs like the Inflation Reduction Act allocate funds to reduce emissions and build climate resilience in healthcare.
- State-Level Support: States may offer subsidies or tax incentives to hospitals implementing renewable energy projects.
- Private Sector Partnerships: Collaborating with industries to co-fund sustainability initiatives.
- Nonprofit and Philanthropy Support: Organizations such as the Commonwealth Fund and Kresge Foundation have launched initiatives focusing on health equity and climate adaptation.
- Community Bond Initiatives: Allow hospitals to secure public investment for climate-proof infrastructure projects.
Accessing these resources often depends on hospitals demonstrating their commitment through detailed climate action plans. Financial backing ensures hospitals can install lifesaving upgrades such as flood-resistant facilities, solar power systems, and robust supply chains.
Collaboration between Sectors
Tackling climate change is not something the healthcare sector can achieve in isolation. Collaboration with environmental agencies, urban planners, and private industry enhances the effectiveness of hospital adaptation strategies.
Key benefits of cross-sector partnerships include:
- Sharing data and research to predict climate impacts on regional healthcare.
- Developing joint response plans for natural disasters, such as wildfires or floods.
- Encouraging green technology development tailored for medical facilities.
- Partnering with environmental advocacy groups to promote policies that reduce emissions.
For example, the National Academy of Medicine’s “Action Collaborative on Decarbonizing the U.S. Health Sector” unites hospitals, policymakers, and environmental groups to reduce healthcare-related carbon emissions. Such initiatives show how collective effort can have a larger, more sustainable impact.
Breaking down silos between sectors fosters innovation and strengthens the capacity of healthcare systems to adapt to a rapidly changing climate. The future of hospitals depends on these cooperative efforts to address shared challenges.
Conclusion
Hospitals face mounting pressure to adapt as climate change intensifies its grip on global health systems. From infrastructure upgrades to sustainable designs and enhanced emergency protocols, the changes required are both urgent and significant.
Healthcare leaders must prioritize these transformations to ensure facilities remain operational and effective during climate-related events. Policymakers and communities also play a key role in supporting hospitals through funding, partnerships, and actionable policies.
Addressing climate risks today safeguards hospitals for the future. What steps can your local facilities take now to prepare?